Radiation Oncology
The Tammy Walker Cancer Center's Radiation Oncology Department, under the direction of Yazan Abuodeh, M.D., provides the most up to date technology and state-of-the-art radiation treatments and is accredited by the American College of Radiology.
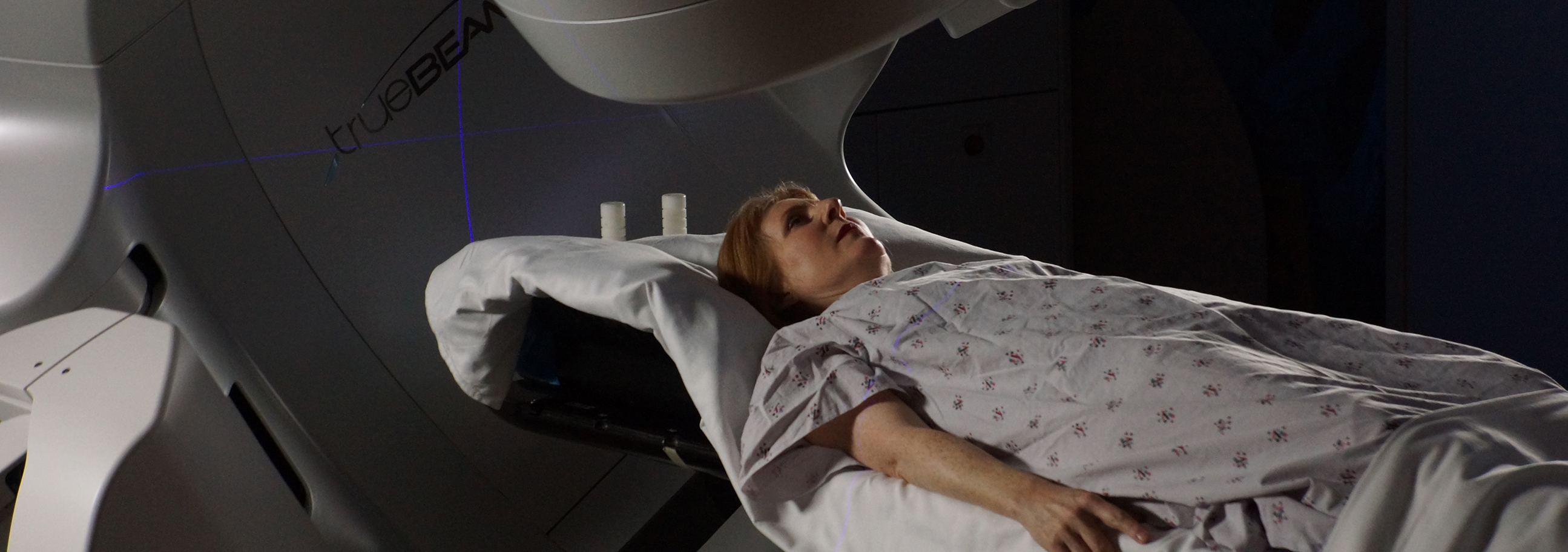
Tammy Walker Cancer Center's advanced radiation therapy technology includes but is not limited to respiratory gating technology, Optical Surface Management System (OSMS) imaging, and six degrees of table rotation for optimal treatment delivery with Varian's TrueBeam® Linear Accelerator radiotherapy system. These technologies allow the team at Tammy Walker Cancer Center to deliver precise, high-dose radiation therapy to small areas of the body, minimizing treatment volumes while sparing healthy tissue. Respiratory gating technology allows treatment to be delivered in tandem with a patient's breathing, and the OSMS imaging system watches the surface of the skin to monitor motion during treatment, increasing accuracy by compensating for minor movements.
Patients throughout the area have found that they can receive excellent cancer care close to home. The Tammy Walker Cancer Center is committed to the fight against cancer and brings some of the best treatments available nationwide to north central Kansas.
- What happens before, during, and after treatment?
- Who are the members of the Radiation Oncology Team?
What happens before, during, and after treatment?
Before you can begin treatment, your doctors must first run tests to determine what type of cancer you have and if it has spread to other parts of the body. Once the diagnosis has been made, you will probably talk with your primary care physician along with several oncology specialists, such as a surgeon, a medical oncologist and a radiation oncologist, to discuss your treatment options. Often, these specialists will work together to help recommend the best treatment for you.
In some cases, cancer will need to be attacked by using more than one type of treatment. For example, if a patient has breast cancer, there may be surgery to remove major portions of the tumor by a surgeon, followed by radiation therapy to destroy cancer cells remaining in or near the breast by a radiation oncologist. At the end of treatment, a patient then might also receive chemotherapy to destroy any cancer cells which have traveled to other parts of the body by a medical oncologist.
Your radiation treatment pathway; an illustrated guide to understanding what to expect
Before Treatment
Consultation With a Radiation Oncologist
If you are considering radiation therapy, you must first schedule a visit with a radiation oncologist to see if radiation therapy is a suitable treatment option for your diagnosis. During the initial visit, your doctor will review your current medical condition, past medical history, past surgical history, family history, medications, allergies and lifestyle. The doctor will also perform a physical examination to assess the extent of your disease and judge your general physical condition. After reviewing your medical tests, including but not limited to: CT scans, MR scans and positron emission tomography scans (PET scans), and completing a thorough examination, your radiation oncologist will fully discuss with you the potential benefits and risks of radiation therapy and answer any questions you might have.
Simulation and Treatment Planning
To be most effective, radiation therapy must be aimed precisely at the same target, or targets, each and every time treatment is given. The process of measuring your anatomy and marking your skin to help your team direct the beams of radiation safely and exactly to their intended locations is called simulation. The simulation process is performed prior to any radiation treatment being given.
During simulation, your radiation oncologist and radiation therapist place you on the simulation machine in the exact position you will be in during the actual treatment. Immobilization devices may be molded or placed on you as part of the plan to help you remain still during treatment. These devices include bag molds, thermoplastic masks, custom molded head rests or other devices constructed for restraining movement during treatment. Under the doctor's supervision, the radiation therapist then marks the area(s) to be treated directly on your skin and/or immobilization devices with a marker or small permanent tattoos. A CT scan will also be taken during simulation to assist with treatment planning. Although simulation is typically only one session, the physician may schedule more than one session depending on the type of cancer and type of radiation therapy being used.
Once you have finished with the simulation, your radiation oncologist and other members of the treatment team review the information they obtained during simulation along with your previous medical tests and use a sophisticated treatment-planning software to help design the best possible treatment plan. After reviewing all of this information, your doctor writes a prescription that outlines the exact course of your radiation therapy treatment.
During Treatment
Treatment Administration
When you undergo external beam radiation therapy treatment, the treatment is painless, like getting an X-ray. The radiation is directed at your tumor from a machine located outside of your body. One of the benefits of radiation therapy is that it is usually given as a series of outpatient treatments and you may not need to miss work or experience the type of recuperation period that can follow other treatments. Treatments are usually scheduled five days a week, every day except Saturday and Sunday. Depending on the type of cancer and its stage of development, there are different treatment scheduling options. With conventional scheduling, the treatments are once a day for five consecutive days. Some patients receive hypofractionation (shorter) radiation therapy, in which radiation treatments are given more than once a day. There is also Stereotactic treatment which ranges from one to five treatments total. Choosing the best treatment scheduling will depend upon the area being treated and what the treatment plan includes. Your radiation oncologist will evaluate, discuss, and recommend the need of treatment and the most optimum treatment schedule for you.
The radiation therapist will administer your external beam treatment following your radiation oncologist's instructions. It will take about 15 minutes for you to be positioned for treatment and for the equipment to be set up. If an immobilization device was made during the simulation, it will be used during each treatment to make sure that you are in the exact same position every day.
Once you are positioned correctly, the therapist will leave the room and go into an adjoining control room to closely monitor you using multiple cameras and a two-way audio system. There is a microphone in the treatment room so you can always talk with the therapist if you have any concerns. The machine can be stopped at any time if you are feeling ill or uncomfortable. The radiation therapist may move the treatment machine and treatment table to target the radiation beam to the exact area of interest. The machine might make noises during treatment which sound like clicking or beeping. These noises are nothing to be afraid of and the radiation therapist is in complete control of the machine at all times. The radiation therapy team carefully aims the radiation to decrease the dose to normal tissues surrounding the tumor. Still, radiation will affect some healthy cells. The time in between daily treatments allows your healthy cells to repair much of the radiation damage.
Most patients are treated on an outpatient basis, and many can continue with normal daily activities. Sometimes a course of treatment is interrupted for a day or more. This may happen if you develop side effects that require a break in treatment. These missed treatments may be made up by adding treatments at the end. Try to arrive on time and not miss any of your appointments. Your radiation oncologist monitors your daily treatment and may alter your radiation dose based on these observations. Also, your doctor may order blood tests, X-ray examinations and other tests to see how your body is responding to treatment. If the tumor shrinks, another simulation may be done for re-planning. This allows your radiation oncologist to change the treatment to destroy the rest of the tumor and spare even more normal tissue.
Weekly Status Checks
During radiation therapy, your radiation oncologist and nurse will see you regularly to follow your progress, evaluate whether you are having any side effects, recommend treatments for those side effects such as medication, and address any concerns you might have. As treatment progresses, your doctor may make changes in the schedule or treatment plan depending on your response or reaction to the therapy. Your radiation therapy team may gather on a regular basis with other healthcare professionals to review your case to ensure your treatment is proceeding as planned. During this session, all the members of the team discuss your progress, as well as any concerns.
Imaging
Depending on your situation, your team will routinely use the treatment machines to take special CT scans or x-rays called port films. This imaging may occur daily or weekly. Your treatment team reviews these images to be sure that the treatment beams remain precisely aimed at the proper target. This imaging is not diagnostic and is not used to evaluate your tumor.
After Treatment
Follow Up
After treatment is completed, follow-up appointments will be scheduled so that your radiation oncologist can make sure your recovery is proceeding as expected and can continue to monitor your health status. Your radiation oncologist may also order additional diagnostic tests. Reports on your treatment can be sent to your other physicians. As time goes on, the frequency of your visits will decrease. However, you should know that your radiation oncology team will always be available should you need to speak to someone about your treatment.
Are there any Side Effects?
Patients often experience little or no side effects from the radiation therapy and are able to continue their normal routines. However, some patients do feel some discomfort from the treatment. Be sure to talk to a member of your radiation oncology treatment team about any problems you may have. Many of the side effects of radiation therapy are related to the area that is being treated. For example, a breast cancer patient may notice skin irritation, like a mild to moderate sunburn, while a patient with mouth cancer may have soreness when swallowing. These side effects are usually temporary and can be treated by your doctor or other members of the treatment team.
Side effects usually begin by the second or third week of treatment, and they may last for several weeks after the final radiation treatment. In rare instances, serious side effects develop after radiation therapy is finished. Your radiation oncologist and radiation oncology nurse are the best people to advise you about the side effects you may experience. Talk with them about any side effects you are having. They can give you information about how to manage them and may prescribe medicines that can help relieve your symptoms.
Who are the members of the Radiation Oncology Team?
While you undergo radiation therapy, a team of highly trained medical professionals will be working together to make sure you receive the best care possible.
Radiation Oncologists
A radiation oncologist is a doctor who specializes in the use of radiation to treat cancer, leads the team, and also oversees your radiation therapy treatments. The radiation oncologist works with the other members of the radiation therapy team to develop your treatment plan and ensure that each treatment is accurately given. Your radiation oncologist will also monitor your progress and adjust the treatment as necessary to make sure the radiation is reaching its target while minimizing side effects. Before, during and after your radiation therapy treatments, your radiation oncologist works closely with other cancer doctors, such as medical oncologists and surgeons, to maximize the radiation's effectiveness. Radiation oncologists have completed at least four years of college, four years of medical school, one year of general medical training, and four years of residency or specialty training in radiation oncology. They have extensive training in cancer medicine and the safe use of radiation to treat diseases and are board certified by the American Board of Radiology.
Radiation Oncology Nurses
Radiation oncology nurses work collaboratively with radiation oncologists and radiation therapists to care for you and your family at the time of consultation, while you are receiving treatment, and during your follow-up care. They will explain the possible side effects you may experience and will educate you on how to manage them. They will assess how you are doing throughout treatment and will help you cope with the changes you may experience. They will also provide support and counseling to you and your family. Radiation oncology nurses are licensed registered nurses or licensed practical nurses. Many registered nurses in radiation therapy have additional accreditation in the specialty of oncology nursing.
Radiation Therapists
Radiation therapists work with radiation oncologists to administer the daily radiation treatment under the doctor's prescription and supervision. They maintain daily treatment records and regularly check the treatment machines to make sure they are working properly. They help you to feel comfortable during the simulation and treatment processes, and will be the ones positioning you during your daily treatments. Radiation therapists go through a two to four year educational program following high school or college. They take a special examination and are certified by the American Registry of Radiologic Technologists and licensed by the KS Board of Healing Arts.
Dosimetrists
Dosimetrists carefully calculate the dose of radiation to make sure the tumor gets enough radiation. Using computers, they develop a number of treatment plans that can best destroy the tumor while sparing the normal tissues. Since treatment plans are often very complex, dosimetrists work with the radiation oncologist and the medical physicist to choose the treatment plan that is right for you. Many dosimetrists start as radiation therapists and then, with very intensive training, become dosimetrists. Others are graduates of one- to two-year dosimetry programs. They are certified by the Medical Dosimetrist Certification Board.
Medical Radiation Physicists
Qualified medical radiation physicists work directly with the radiation oncologist during treatment planning and delivery. They oversee the work of the dosimetrist, and help ensure that complex treatments are properly tailored for each patient. Medical physicists are responsible for developing and directing quality control programs for equipment and procedures. Their responsibility also includes making sure the equipment works properly by taking precise measurements of the radiation beam and performing other safety tests on a regular basis. Qualified medical physicists have doctorates or Master's degrees. They have completed at least four years of college, and then generally two to four years of graduate school. They also typically have one to two years of clinical physics training. Medical physicists are certified by the American Board of Radiology or the American Board of Medical Physics.
During your treatment, you may work with a number of other healthcare professionals while undergoing radiation therapy. These specialists ensure that all of your physical and psychological needs are met during your treatment.
Additional members of the team
Nutritionists
Nutritionists, also called dietitians, work with patients to help them maintain proper nutrition during their treatments. They will help you modify your dietary plan if the side effects of treatment are affecting your appetite and what you can eat. They can provide recipes, menu suggestions and information on ready-to-use nutritional supplements. They address dietary issues and current developments that may affect cancer treatment outcomes.
Social Worker
Social workers help coordinate patient care and connect patients and families to resources both at the clinic and in the community. The social worker can provide a new patient orientation, coordinate transportation and lodging, help navigate Medicaid and Social Security Disability as well as refer to community resources based on individual need.
Physical Therapists
Physical therapists use therapeutic exercises to ensure that your body functions properly while you are undergoing treatment. These exercises are used to help manage side effects, alleviate pain and keep you healthy.
Dentists
Dentists may be involved in the care of patients who are receiving radiation for oral or head and neck cancers. They will help prevent the radiation from damaging the healthy areas of your mouth and oral cavity, and may recommend that you have preventive dental work prior to radiation. They will also help you manage oral complications of cancer therapy, such as dry mouth. A dental hygienist may also perform these services under the supervision of a dentist.